The Covid-19 crisis has stretched already limited mental health support in low- and middle-income countries. Interventions that make use of accessible technology may offer scalable, low-cost solutions in resource-poor settings.
The Covid-19 pandemic has taken a heavy toll on people’s mental health around the world. While the physical health effects – particularly the four million lives that have been lost globally – may be more evident, the impact on mental wellbeing has still been significant.
Around 80% of people with mental health problems reside in low- and middle-income countries (Rathod et al, 2017). Many of these countries lack adequate mental health resources and have been unable to offer significant support to mitigate the effects of job loss, income shocks and food insecurity during the pandemic – all of which may be drivers of poor mental health (Daly et al, 2020; Rahman et al, 2021).
Further, mental health problems are often not considered health issues that require medical attention in some low- and middle-income countries. This affects the resources that are allocated to mental health treatment. Indeed, around 75% of people with mental disorders in developing countries never receive any treatment (Kovacevic, 2021).
On average, countries spend only 1.7% of their health budgets on mental health (Ridley et al, 2020). But there is a significant gap between high- and low-income countries. For many high-income countries, the health budget allocated to mental health is over 3%, while for developing countries it is less than 0.5%. Crucially, in developing countries the overall health budgets are often already much lower.
Access to trained mental health professionals is also limited in developing countries. For example, in 2016, India had 0.29 psychiatrists working in the mental health sector per 100,000 population. Similarly, South Africa had 1.52 and Brazil 3.16. This compared with 10.54 in the United States, 20.91 in France and 48.04 in Norway (World Health Organization, 2016).
Such already limited services have been further stretched by the Covid-19 crisis, which has increased demand for mental health support. At the same time, the World Health Organization reported in October 2020 that the pandemic had ‘disrupted or halted critical mental health services in 93% of countries worldwide’ (WHO, 2020).
Financial concerns, poverty and worries over one’s health or that of a loved one – in settings where there are fragile healthcare systems, high population density, lack of resources, and a poor social safety net – all exacerbate this problem.
Poor mental health support can lead to worse socioeconomic outcomes (Angelucci and Bennett, 2021). This can happen as a result of fatigue, disrupted sleep and impaired cognition, which may reduce labour supply and productivity and, thus, may negatively affect income. Lack of access to mental health support can leave people in developing countries vulnerable to pervasive and serious psychological distress, particularly those who live in poverty (Ridley et al, 2020).
What does evidence from economic research tell us?
Experts highlighted the potential psychological impact of the pandemic at the onset of the outbreak. They emphasised the necessity of planning, research and supportive measures to provide mental health support to Covid-19 survivors and people that are vulnerable to mental health problems (Galea et al, 2020; Holmes et al, 2020).
Evidence from previous health crises has shown prolonged isolation could lead to several psychological problems such as acute stress, post-traumatic stress disorder, psychological distress, depressive symptoms, and other emotional disturbances (Brooks et al, 2020). The fear of Covid-19 infection and death can also lead to aggravated anxiety, anger, confusion and post-traumatic symptoms (Ornell et al, 2020; Mukhtar, 2020; Pakpour and Griffiths, 2020).
Additionally, with an extremely contagious disease, in settings where awareness of the diseases may be affected by misinformation, there is an increased likelihood of stigmatisation, both in cases of real or false association with the disease (Islam et al, 2021; Siddique et al, 2020).
To combat such effects, organisations such as the World Bank have supported initiatives that deliver mental health interventions during the pandemic. Several countries such as Cambodia, Guatemala, Lesotho, Liberia, Mali, Marshall Islands, Morocco, Niger, Nigeria, Republic of the Congo and Sri Lanka incorporated provision for mental health in their health care programmes to combat the potential psychological effects of Covid-19 (Kovacevic, 2021).
In addition to the immediate health impact of Covid-19, its economic effects have also hit low- and middle-income countries hard. In developing countries, medium- and small-scale businesses have been massively affected, while support from the governments is often inadequate. A significant portion of the population in these countries is reliant on the informal sector where people have experienced income loss and food insecurity (Ahmed et al, 2021; Beam et al, 2021; World Bank, 2020).
These financial burdens and uncertainty surrounding future income can affect people’s mental wellbeing. Alongside health concerns, misinformation and stigma, financial concerns have also contributed to declines in mental wellbeingduring the pandemic.
Women are more likely to be affected by the consequences of the pandemic, including mental health problems, due to their disadvantaged socioeconomic position relative to men, the heavier burden of daily chores, their critical role in managing household food shortages, and their care responsibility for children and elderly family members.
A gender analysis of the impact of Covid-19 published by United Nations (UN) Women found that in Bangladesh, women performed over three times more unpaid care work than men pre-pandemic (United Nations Women, 2020). It also showed that compared with men, women experienced higher rates of symptoms of depression and anxiety during the pandemic.
Another study reported that the average Patient Health Questionnaire (PHQ) -9 score, which measures depression severity, is 8 (mild depression) for women in Bangladesh, while the average for men is only 3 (minimal depression) (Beam et al, 2021).
Similarly, in India, women reported relatively more mental stress than men (Afridi et al, 2021). One possible reason being gender norms at the household level. Attitudes toward women’s roles, decision-making, and domestic violence may all play an important role in the reporting and incidence of poor mental health conditions among women in developing countries.
Studies in developed countries have also produced similar findings. For example, in the UK, research has shown that women experienced significantly higher mental distress than men irrespective of their ethnicity (Proto and Quintana-Domeque, 2021). The reason being that women are more vulnerable within households in both developed and developing countries. Therefore, policies prioritising the vulnerabilities of women are likely to play an important role in improving their mental heath during the pandemic.
What might be a potential response?
Addressing mental health problems in low- and middle-income countries is challenging for many reasons. These include limited resources and skilled workforce, rural-urban divides in access to care and stigma around mental illness (Dsouza et al, 2020).
Nevertheless, there are some examples of effective mental health support from low- and middle-income countries. For example, tele-consulting and videoconferencing psychiatry, along with the use of non-specialised trained mental health workers, have been effective in treating common mental health issues in India (Thara, 2012). A randomised controlled trial in Brazil found videoconferencing to be helpful in reducing the severity of depression among patients with mild depression (Hungerbuehler et al, 2016).
Further, during the Covid-19 pandemic, Building Resources Across Communities (BRAC) implemented a tele-counselling service in Bangladesh. This service appears to be critical during a crisis like Covid-19 given that there are about 200 psychiatrists and 600 psychologists and psychotherapists in total in the country, while around 11,000 people commit suicide every year due to mental disorders (Mariam and Chowdhury, 2020).
A trial in Iran has also shown bibliotherapy, an approach that uses information brochures and literature to support mental health, to be an effective tool to help patients suffering from depressive symptoms (Taleban et al., 2016).
In Bangladesh, one study trialled a four-module tele-counselling intervention for women in rural areas (Vlassopoulos et al, 2021). The four modules covered the following mental skills:
- behavioural: problem-solving, behavioural activation, relaxation, and exposure;
- interpersonal: identifying/eliciting support and communication skills;
- emotional: linking affect to events and emotional regulation and processing; and
- cognitive: identifying thoughts, insight building, distraction, and mindfulness.
They also followed the Covid-19 mental health and psychosocial support guidelines assembled by the International Federation of Red Cross, the World Health Organization, and wider mental health research to include context-specific support, including:
- Tools to combat fear: general awareness on Covid-19, modes of transmission, health guidelines to prevent infection, and potential sources of support.
- Coping with stress: breathing exercises and techniques to manage stress, stressful thoughts and emotional outbursts.
- Self and childcare: re-emphasising Covid-19 related health guidelines, self-care during pregnancy, caring for young children and someone unwell with Covid-19-like symptoms, and seeking medical help in an emergency.
- Communication: help with staying connected with loved ones and neighbours via mobile phone, avoiding Covid-19 related rumours and blaming or ostracising people for contracting the disease, and offering a one-off phone credit to encourage communication with relatives/neighbours.
This support, delivered by trained women para-counsellors, appears to have reduced stress levels and the severity of depression (as shown in Figure 1). It also improved a number of secondary outcomes such as happiness, life satisfaction, future aspirations, household-level food insecurity, time-intensive parental investment, gender empowerment, attitudes toward gender norms and attitudes toward intimate partner violence. The effects are stronger for women that had high stress at baseline, are relatively older, and are from lower-income households.
Figure 1: Distributions of stress and depression by treatment status
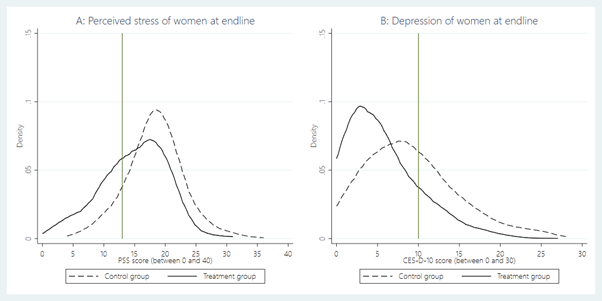
Source: Vlassopoulos et al, 2021
What worked?
Several interventions designed to address the mental health situation during the pandemic suggest that initiatives should consider:
- Using short sessions to avoid adding to the participants’ daily burden of chores.
- Employing locally recruited para-counsellors to engage with the participants effectively.
- Adopting an empowering approach based on skill and knowledge building, instead of identifying participants as “mental patients”.
- Making use of low-cost technology to provide services to hard-to-reach communities, for example, telephone-based interventions.
What does all this mean for policy?
Given the constraints of allocating limited resources in developing countries – particularly during a health crisis such as the Covid-19 pandemic – low-cost scalable solutions will be important to address the worsening mental health situation. Interventions that support hard-to-reach populations, including those living in rural communities, will also have a wider impact. Examples include the use of text messaging, video conferencing, and tele-counselling.
The findings from a number of studies suggest that a brief tele-counselling intervention using non-specialised counsellors could be effective in ameliorating the mental health of women in a resource-poor context. The remote and empowering nature of the intervention and the low cost of implementation makes it scalable and applicable in similar contexts, where providing mental health support is otherwise challenging during times of crisis.
With the delta variant spreading and lockdowns being enforced or extended in many countries, mental health problems are likely to worsen due to a lack of resources and experts, as well as poor mental health support mechanisms.
The pandemic has highlighted the vulnerability of people and the need for additional mental health support around the world. This momentum can be seen as an opportunity to address the unmet needs of one of the most vulnerable groups – women living in rural areas – by considering effective ways of investing in mental health support to improve their overall wellbeing.
Where can I find out more?
- Covid-19 Bangladesh Rapid Gender Analysis: Report from UN Women on the pandemic’s effect on pre-existing structural social and economic vulnerabilities among women, girls and diverse gender groups
- Mental health: lessons learned in 2020 for 2021 and forward: World Bank blog on global mental health
- Global Mental Health: Some Perspectives on Challenges and Options for Scaling Up Response: Suggestions for a sustained global response to mental health issues.
- Covid-19 disrupting mental health services in most countries: World Health Organization article on the need to increase investment in mental health resources
- On World Mental Health Day: A call to invest in interventions for young people: Blog from the World Bank
Who are experts on this question?
- Sonia Bhalotra, University of Warwick
- Pim Cuijpers, Vrije Universiteit Amsterdam
- Johannes Haushofer, Stockholm University
- Vikram Patel, Harvard University
- Gautam Rao, Harvard University
- Frank Schilbach, MIT