Was the government doing enough to ‘protect the NHS’ in the years leading up to the pandemic? The UK needs a rigorous assessment of whether a national health service that is always operating at full capacity can cope with unexpected shocks like Covid-19.
Protecting the capacity of NHS services is seen as vital for dealing with the Covid-19 pandemic. The message from the UK government during the worst phase of the outbreak was to ‘stay home, save lives, protect the NHS’. But was the government doing enough to protect the NHS in the years leading up to this pandemic?
Over the last decade, the healthcare sector has not had adequate public funding for it to grow and develop. It has been affected by austerity measures and uncertainty over Brexit. The UK’s ageing population has created additional demand for healthcare services and, coupled with stagnant government spending, this has increased the pressure on service provision.
What does evidence from economic research tell us?
Economic research is helpful in highlighting the relationship between healthcare spending, staffing and health outcomes. Evidence suggests that healthcare spending is correlated with improvements in certain health outcomes in the UK (Martin et al, 2008; Bokhari et al, 2006). Similar results are also found for other countries. For example, there is a significant negative correlation between hospital spending and mortality in the United States (Doyle et al, 2015; Doyle, 2011) – that is, the higher the spending, the lower the mortality.
Other researchers have used disruptions to healthcare provision to measure the impact on health outcomes (Propper et al, 2020). Gruber and Kleiner (2012) find that nurses’ strikes in the United States increase in-hospital mortality by about 18%. It is worth noting, though, that due to the complex relationship between healthcare spending and health outcomes, and the difficulty in measuring health outcomes, many of these studies show mere correlation rather than establishing a causal relationship.
An important determinant of a thriving healthcare system is human resources. Studies show that there is also a positive correlation between health outcomes and the density of healthcare professionals. For example, it has been shown that a higher number of doctors and nurses per 1,000 people improves health outcomes (Anand and Bärnighausen, 2004).
Economic research is also helpful for understanding the incidence and consequences of shortages in healthcare labour markets (for example, Nicholson and Propper, 2011). It can offer insights on how to counteract human resource shortages in key sectors of the economy, including through employing foreign workers or investing in training domestic employees.
Writing here at the Economics Observatory, Buchan and Shembavnekar (2020) note that achieving self-sufficiency in nursing is unlikely to be feasible in the short term by relying on domestic nurses only. Reliance on foreign nurses also brings its own challenges in terms of global competition in recruitment and retention, and the potential consequences of immigration.
Economic research on immigration helps us to understand the role of migration in the labour market (for example, Dustmann et al, 2005). It also highlights the drivers and barriers to migration for economic migrants, such as the implications of the referendum on the UK’s membership of the European Union (EU) for immigrants’ intentions to stay or leave the country (for example, Falkingham et al, 2018).
Related question: What will coronavirus mean for self-sufficiency in nurse numbers?
Has expenditure on healthcare been adequate?
Examining the patterns and trends in healthcare spending over the past few years shows that the UK has had higher healthcare expenditure as a share of GDP than the OECD average, but lower healthcare spending per person (second lowest among G7 countries) – see Figure 1. UK expenditure lags behind most West European and Nordic countries. The highest spenders have been France, Germany and the United States.
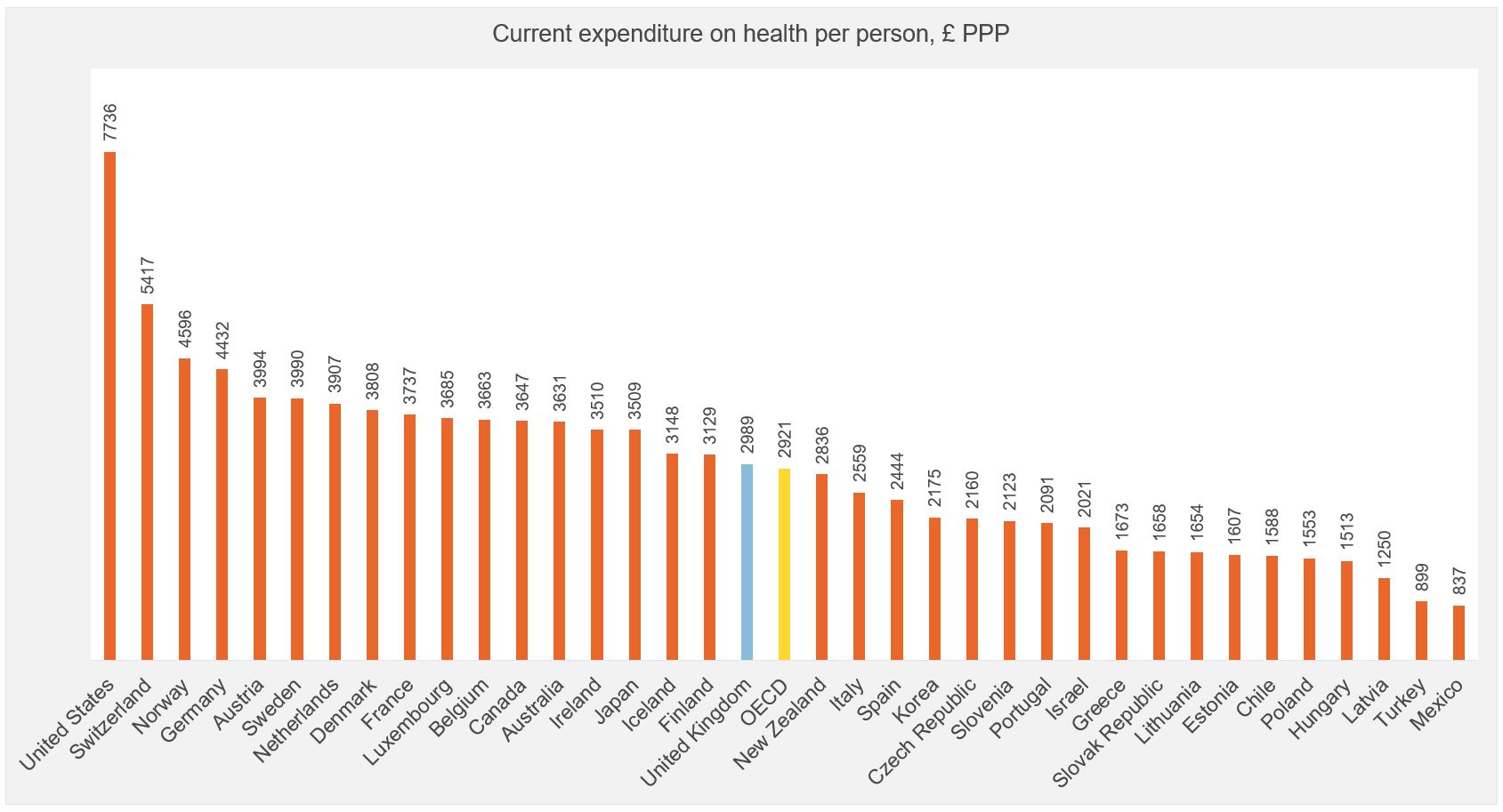
Since 2010, the real average annual growth in UK government expenditure on the health sector has been only 1.3% – see Figure 2. Austerity measures are the primary factor behind this low growth. At the same time, demand for healthcare services has been increasing, not least due to an ageing population, with 18% of the population over 65 years of age in 2018 (see, for example, Johnson et al, 2018; and Ghazaryan et al, 2020).
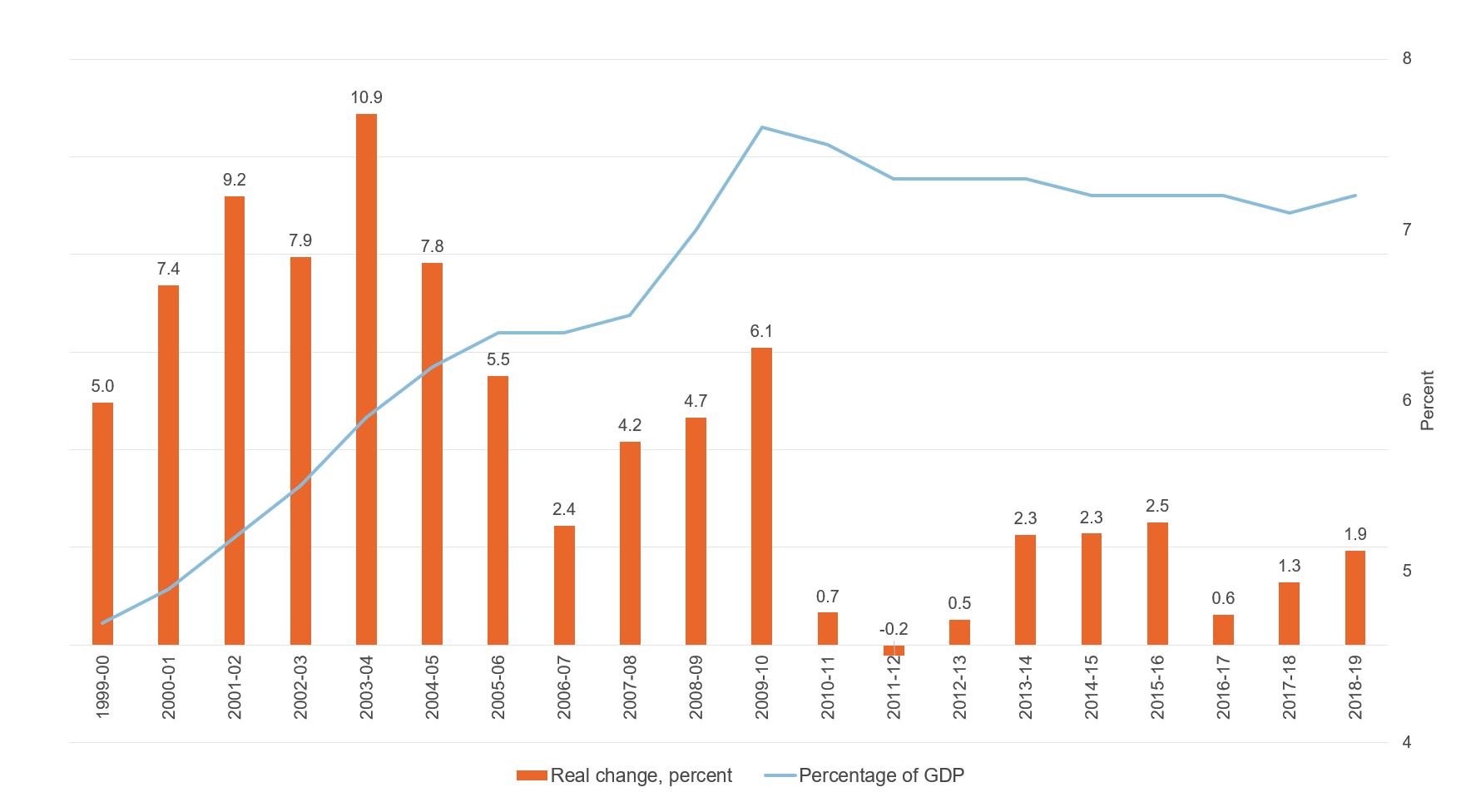
A decline in real-terms spending over the last decade has inhibited the growth of the NHS workforce. The number of doctors and nurses per 1,000 population in the UK is much lower than in other OECD countries, and there is relatively low hospital bed availability – see Figure 3. In fact, the UK has much fewer doctors (2.8) and nurses (7.8) per 1,000 people compared with the OECD average. The number of doctors per 1,000 people is the second lowest among EU countries.
Overall, the evidence demonstrates that in the last decade, the NHS has not been provided with adequate public funding to enable it to grow and meet the increasing demand for healthcare services. During this time, however, NHS managers have been under pressure to reduce waste and increase efficiency gains through increasing productivity and savings.
As a consequence, productivity in the healthcare sector in the UK has been growing faster than the rest of the economy since 2011, while hospital occupancy has often been around 90%. This raises the key question of whether it is sensible for the NHS to be operating close to full capacity. Worryingly, as witnessed during the spread of the pandemic in the spring of 2020, a major constraint has been the lack of NHS capacity to cope with demand for care.
Figure 1: OECD comparison of health expenditures
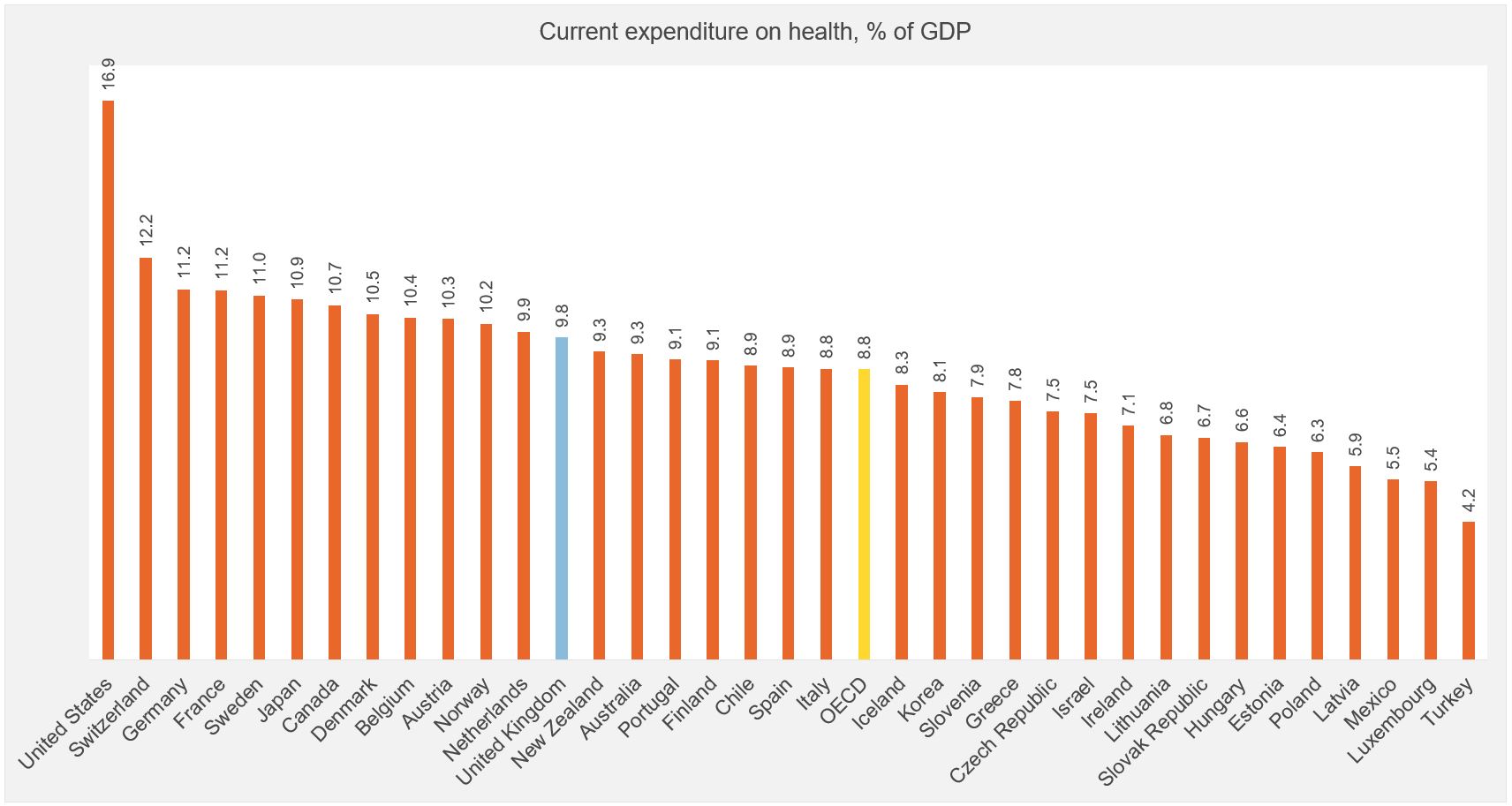
Source: OECD Health Statistics 2019 and Office for National Statistics.
Note: This shows current expenditure (all financing schemes) on healthcare as a percentage of GDP and in pound sterling purchasing power parity (£PPP) per person. The figure for current expenditure as a percentage of GDP is for 2018, while the figure for current expenditure in £PPP per person is for 2017.
Figure 2: Dynamics of UK public sector expenditure on healthcare
Source: HM Treasury Public Expenditure Statistical Analyses 2019.
Note: This shows the dynamics in real change in public expenditure on the health sector, as well as expenditure as a percentage of GDP. Real change is calculated from nominal expenditure figures, adjusted to 2018/19 price levels using GDP deflators from the ONS. Real changes are calculated as annual percentage change (growth/reduction) in expenditure in real terms.
Figure 3: OECD comparison of healthcare resources
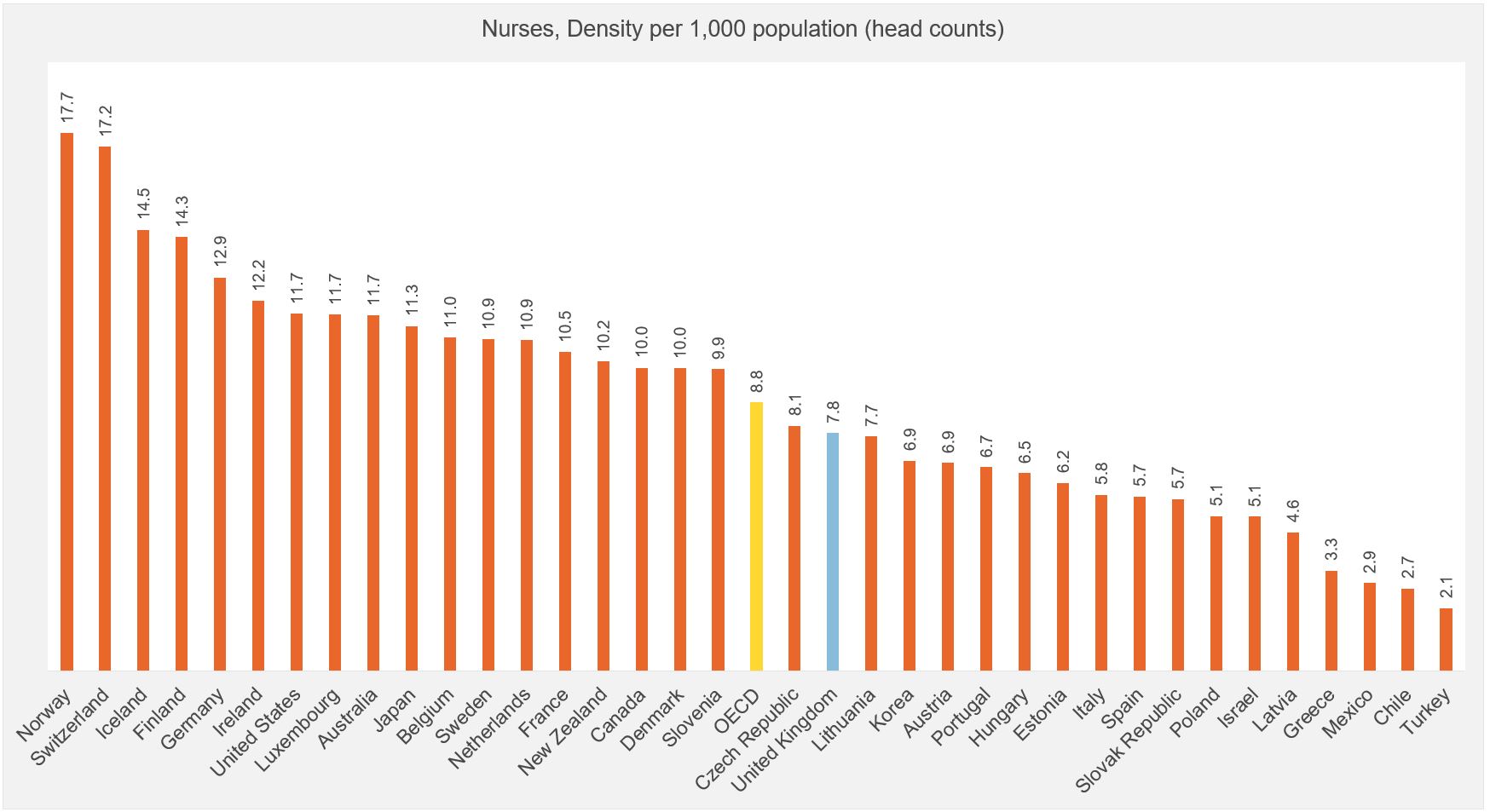
Source: OECD Health Statistics 2019.
Has the NHS been empowered?
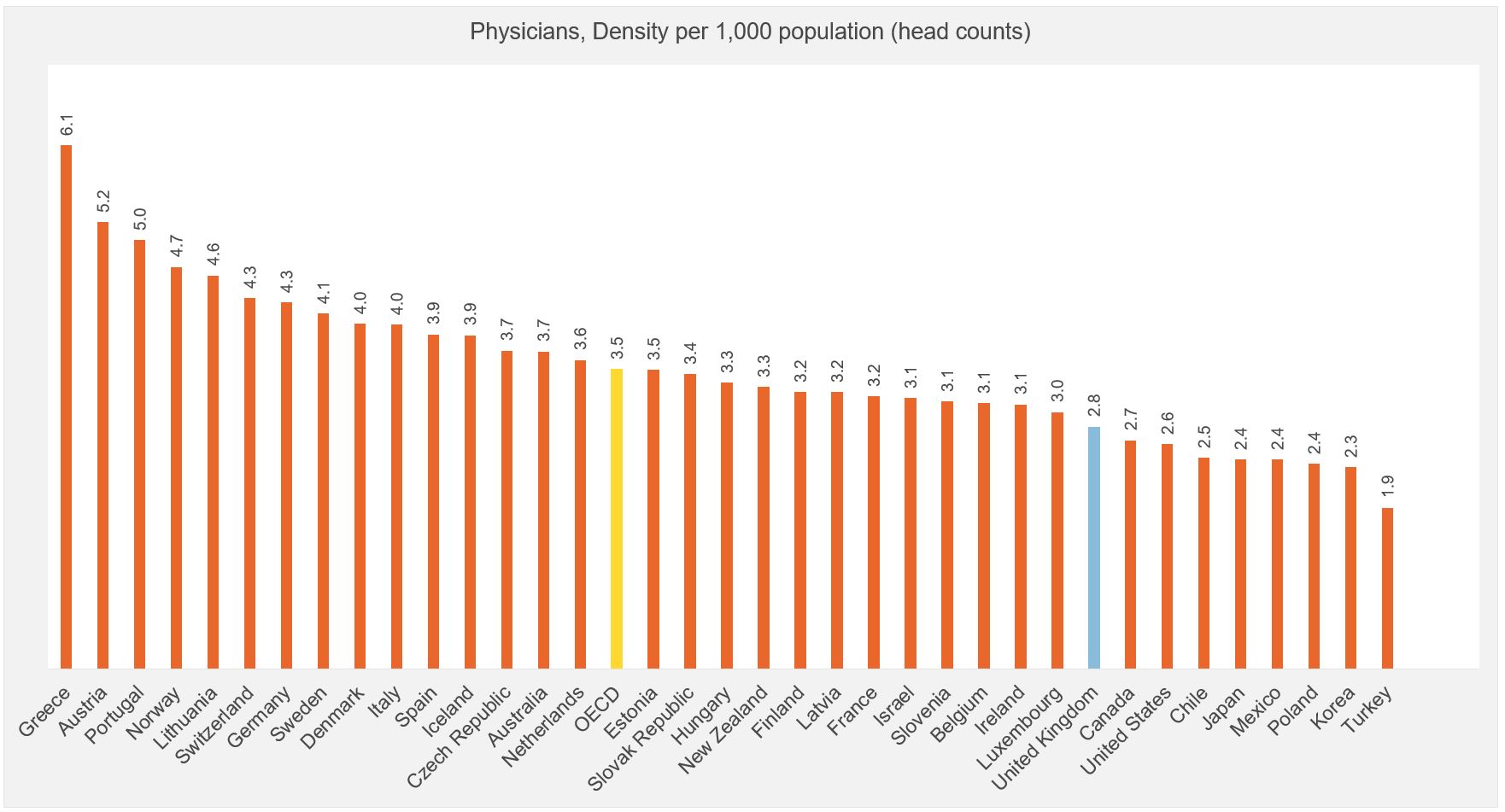
According to the Office for National Statistics (ONS), in 2019, the NHS employed around 1.2 million people. Since 2010, the number of NHS professionally qualified staff has grown annually by 1% on average, bringing overall growth during this period to around 10% – as shown in Figure 4.
The growth has been driven by an increase in the number of doctors, masking a very low annual increase in nurses at only 0.3% per annum, with a cumulative growth of about 4%. Importantly, the increase in the health workforce has failed to keep up with population growth, and therefore does not translate into more doctors and nurses per head.
The UK has relied on foreign-born doctors and nurses more than other OECD countries. The importance of the non-UK health workforce has been steadily increasing since the early 2000s, and by 2019, over 20% of the workforce was composed of foreign workers. Yet since the vote for Brexit, the number of EU doctors has been increasing at a slower pace than previously, while the supply of EU-born nurses has dropped.
Immigration policies play a critical role in helping to fill shortages in the health professional workforce. A wide variety of policies and issues directly and indirectly affect the attraction and retention of healthcare professionals (see Buchan and Shembavnekar, 2020). The NHS workforce is very diverse and international, an aspect that has attracted public and media attention during the Covid-19 pandemic.
Black, Asian and minority ethnic (BAME) groups are overrepresented in the NHS. Around 49% of doctors and 27% of nurses in England are of BAME background, while the BAME population constitutes around 14% of the UK population, highlighting the contribution of BAME communities as key health workers.
Despite the clear contribution of healthcare professionals to ensuring an effective NHS, there have been growing concerns about low pay and inappropriate working conditions, both of which it is essential to address in order to ensure an empowered NHS workforce.
The future of a national health service that is fit for purpose in the era of ageing populations depends on attracting and retaining an adequate number of trained nurses and doctors. According to statistics from the Higher Education Statistics Agency (HESA), there has been an increase in the number of UK-born students enrolling in medicine and dentistry in the last five years.
But the number of newly enrolled UK-born students in nursing has been declining, suggesting that the UK might face an imminent shortage of nurses. This decline is likely to be attributable to the government’s abolition of the student grants for nurses in England and Wales in 2017. Note, however, that grants for nursing students have been reinstated from September 2020.
Figure 4: Cumulative change in the number of medical professionals, the UK population and the ageing population of Great Britain
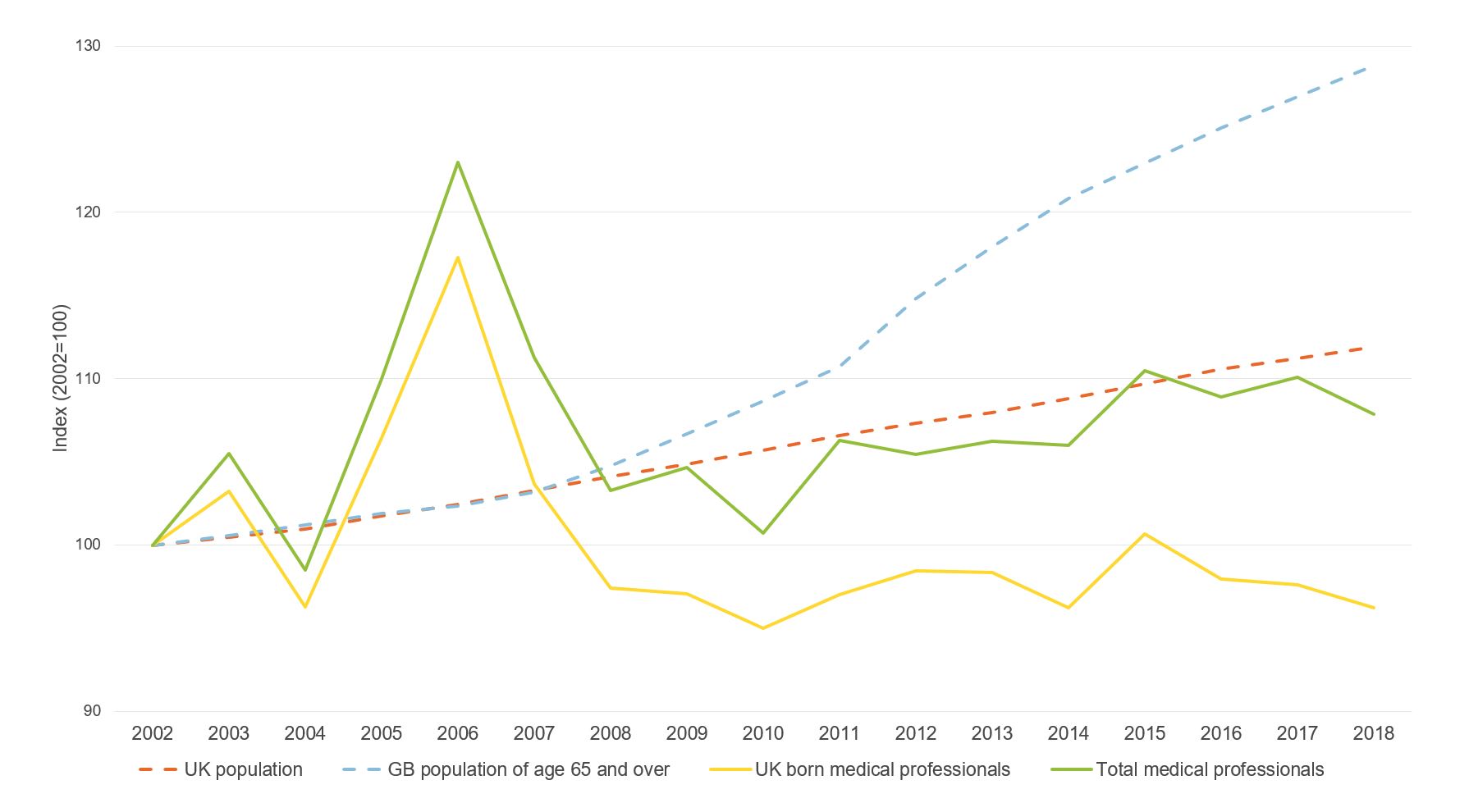
Source: Labour Force Survey and ONS.
Note: This shows the cumulative change in UK-born and non-UK-born medical professionals (including hospital and medical practice workers), the UK population and the population aged 65 and over in Great Britain. Person weights are applied in calculating the change in the number of medical professionals.
What should policy do?
At this critical time, it is important for the UK government to ‘protect the NHS’ by ensuring that spending on healthcare is growing in line with an ageing population. At the same time, there is a need for a rigorous and comprehensive assessment of the implications of a national health service that is always operating at full capacity for its ability to cope with unexpected shocks such as Covid-19.
It will also be vital to nurture more medical students through training and, crucially for nursing students, through funding. Of course, medical workforce training takes time. While nurses starting their education today will be entering the workforce in three to four years, it takes much longer for doctors to acquire the necessary education and practice.
It is therefore important that temporary shortfalls in the domestic workforce are well managed. The UK government needs to attract and retain foreign doctors and nurses to enable the country to cope with the Covid-19 pandemic and the Brexit transition – and to deal with potential future global health emergencies.
Looking ahead, as global competition for healthcare professionals increases, innovative global initiatives will be needed. One example of such policy proposals is the Global Skill Partnership (see, for example, Clemens, 2015), which envisions linking skill formation and skilled migration. In essence, destination countries could agree to provide technology and finance to train potential migrants with targeted skills in the countries of origin.
This approach would have the advantage that training provision would be typically cheaper in the countries of origin, but at the same time, it would provide potential migrants with the skills needed to be employable in destination countries. For healthcare workforces, this policy would provide mutual benefits: to origin countries as they benefit from skill formation; and to destination countries, which would be able to manage migration and fill skill shortages in their health labour markets.
It is clear that the Covid-19 pandemic is changing the NHS and other healthcare systems across the globe. For example, doctors are replacing in-person consultations with telephone calls with patients, and prescribing medication based on telephone and video discussions.
But how far will the changes go and how persistent will they be? Advances in artificial intelligence are likely to start assisting and complementing healthcare workers and even substituting certain roles in medical care; robotic nurses, for example, have been operating for several years in Japan.
In conclusion, it is important to ensure that the NHS is well prepared to deal with current and future pandemics – to protect the NHS to save lives.
Where can I find out more?
- Empowering the NHS: Challenges for the pandemic: Armine Ghazaryan, Corrado Giulietti and Jackline Wahba examine the preparedness of the NHS in the decade leading up to the pandemic in this briefing from the Centre for Population Change.
- NHS Workforce Statistics: The key source of data on UK nurse numbers and vacancies as well as data on other healthcare workforce categories.
- OECD Health Statistics 2020 – Health Workforce Migration: OECD statistics on the number and proportion of foreign-trained nurses by country of origin.
- The wider impacts of the coronavirus pandemic on the NHS: An April 2020 briefing by Carol Propper, George Stoye and Ben Zaranko, published by the Institute for Fiscal Studies.
- What will coronavirus mean for self-sufficiency in nurse numbers? James Buchan and Nihar Shembavnekar, Economic Observatory, September 2020.
Who are experts on this question?
- James Banks, Professor of Economics at the University of Manchester and Co-Director of the Centre for the Microeconomic Analysis of Public Policy at the Institute for Fiscal Studies
- Carol Propper, Professor of Economics at Imperial College Business School in the Department of Economics and Public Policy
- George Stoye, Associate Director at the Institute for Fiscal Studies
- Carlos Vargas Silva, Director of the Centre on Migration, Policy and Society (COMPAS) and Associate Professor at the University of Oxford









































