Limited supplies of Covid-19 vaccines mean that hard choices need to be made. There have been a variety of different national strategies for deciding who should be priorities for the first doses. Each method of allocation raises health, economic and ethical issues.
Since the first announcement that a vaccine effective against Covid-19 had been developed, it has offered hope as a way out of the pandemic. New vaccines have been approved since then, but still there are not currently enough vaccines to go round.
When considering how to allocate limited numbers of doses, there are questions of priority within countries as well as across countries. Here, we concentrate on the former – in other words, who among a country’s population should receive the vaccination first?
Any strategy on who should be priorities for vaccinations will have implications for health and mortality (Hogan et al, 2020). There are three general effects of vaccines:
- Effectiveness: vaccines affect the probability of individuals becoming infected.
- Transmission: vaccines affect the probability of those who become infected passing it on to others.
- Protection: vaccines affect the severity of symptoms in those who become infected.
Consequently, decisions about priorities must consider which groups will be most severely affected by the disease in terms of health outcomes, and which groups are most likely to transmit the disease to others.
How are vaccines currently being allocated?
The vast majority of countries have adopted a public allocation system for Covid-19 vaccines rather than letting individuals buy the jabs. But in India, vaccines can be purchased by eligible individuals at a subsidised price. The eligible group currently consists of the over-60s and those 45-60 years old with existing health concerns, but it will be anyone over 45 years of age from 1 April.
Similarly, vaccines were initially available in China at a cost even to high-risk workers as part of a national programme, but they are now free. The uptake of vaccines remains slow in both countries, and in India, about 6.5% of vaccines are being wasted.
In countries where governments are administering vaccines, a strategy of priorities is required to decide who gets their dose first. There are five primary goals for allocating them: protection of the most vulnerable; protection of the healthcare system; protection of key workers (other than those in healthcare); protection of the working population; and equity (Arras, 2005).
Protecting the vulnerable
Many countries, including the UK, have made a priority of vaccine distribution to those who are most vulnerable to the disease. As the mortality from Covid-19 is higher among older people, age has been a primary determinant in this strategy – see Figure 1. In terms of medical ethics, this strategy is maximising benefits by minimising the number of lives lost (Emanuel et al, 2020).
Figure 1: Deaths within 28 days of positive test by date of death age demographics
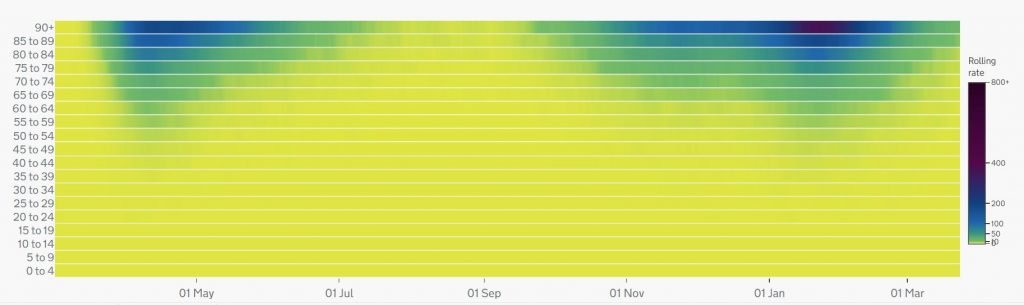
Source: Office for National Statistics
In several countries, mortality from coronavirus has been very high in care homes. Their set-up has meant that isolating the infected from the non-infected is difficult, and as residents are more likely to be vulnerable to the disease, mortality is very high. Thus, countries such as the UK, the United States, France, Spain, Sweden and Canada have made a priority of vaccinations in care homes. But this may not affect transmission of the disease as residents are already largely isolated.
In the UK, the Joint Committee on Vaccination and Immunisation (JCVI) examined other considerations but ultimately adopted an age-based strategy that also took account of other medical conditions, as this offered a clear implementable strategy. As the JCVI’s Lim Wei Shen said, ‘The evidence is clear that the risk of hospitalisation and death increases with age… Following an age-based programme will be simple, and simplicity has been one of the cornerstones of the current programme in terms of speed and its success’.
Which groups are considered elderly varies across countries – from those over the age of 60, for example, in Latvia and the Netherlands, and above 70 in countries such as Estonia and Sweden, to a defined graduated policy as in the UK.
Israel, which has hadone of the fastest vaccination programmes, has made a priority of people aged over 60 and those at risk due to pre-existing medical conditions. Belgium also took other health issues into account, but the difficulties with implementation have led to calls for a simpler age-based strategy.
With an age-based strategy, there are significant differences within the population to consider. Life expectancy at birth varies by 11.3 years across the UK: from 87.2 years for women and 84.9 for men in Westminster to 78.5 for women and 73.6 for men in Glasgow. This is a striking difference when we consider that the over-70s were priority group 4 in the UK.
These variations are linked to socio-economic status. Inequality data show that life expectancy in an area decreases with relative deprivation. There are also differences across ethnic groups on health-related quality of life above 55 years of age. The elderly in 15 out of 17 ethnic groups have worse health outcomes than white British (Watkinson et al, 2021).
Minority groups in many countries, including England and Wales, have had higher mortality rates from Covid-19 than the rest of the population controlling for age and health conditions – see Figure 2. These differences between ethnic groups also apply to the new strain of the Covid-19 virus.
Figure 2: Rate of death involving Covid-19 by ethnic group and sex relative to the white population for people in private households, England, 2 March to 28 July 2020
Source: Office for National Statistics
Disparities by socio-economic background and ethnicity have not been factored into the vaccination strategy in the UK. Adopting only an age-based list will increase these disparities.
In contrast, Australia has a lower cut-off (55 years) for Aboriginal and Torres Islanders than the rest of the population (70 years). Canada has also made a priority of its indigenous minority population.
Protecting healthcare
A second allocation strategy focuses on healthcare, specifically vaccinating workers in the sector. In some cases, this has also included those responsible for providing home care. While this approach protects health workers and carers themselves, the main consideration is their ability to prevent severe illness or the death of others. There is obvious concern that if there are infections of healthcare workers, then the healthcare system could be overwhelmed.
Consequently, Italy, India, the Netherlands, Russia, France, Germany and the United States have all made a priority of these individuals. In India, vaccines were given to others only after healthcare workers had received theirs. The Korean policy is to vaccinate frontline medical staff treating Covid-19 patients first, and then the elderly and healthcare workers. The UK has also made a priority of the vaccination of frontline health and social care workers alongside the elderly.
Severe infections among healthcare workers are generally lower than for non-healthcare workers, and their mortality from coronavirus is in line with trends in the general population (Kim et al, 2020; Bandyopadhyay et al, 2020). Therefore, the rationale for making a priority of the vaccination of these individuals is not their own risk factors but rather their ability to help or save others – what is known as their instrumental value (Emanuel et al, 2020).
Protecting other key workers
Several countries have made a priority of non-medical key workers. The reasoning for vaccinating this group first is that if they were to become infected, their absence from the workforce would have severe social and economic consequences.
The definition of key workers varies across countries. For example, Singapore has reserved 5% of vaccines for critical workers, a group that includes airline crew and maritime workers.
In the United States, the Centers for Disease Control and Prevention (CDC) issued guidelines that include key workers in the priority list. But each state follows its own policy, such that in New York state, school teachers and university professors who have to teach in person (laboratory or clinical work) are also high priority, while Texas gives priority to a much smaller group of key workers.
People working in food supply, distribution, public services and utilities are included in several countries, including France and Germany. China made military personnel and diplomats priorities, as well as employees of the telecoms giant Huawei. People who are in the 18-60 age group working in healthcare or going abroad can also register and get vaccinated.
Other countries, such as India, give high priority to government employees. In Russia, healthcare workers, teachers and social workers are on the priority list as they have the highest risk of exposure to infection.
In this approach, consideration is given to those who are essential to keep the country running, as well as those who are exposed to greater risks of infection through their work, such as teachers and social workers.
Protecting the working population
Governments deciding their vaccine allocation strategies have to consider the balance between protecting the working population and those who are most vulnerable. Few Western countries have chosen to focus on the working population, perhaps as they generally have a higher proportion of elderly in the population and thus face higher mortality risks.
But this approach has been pursued in some Asian countries that have younger populations. For example, Indonesia has made a priority of vaccinating the working age group of 18-59 year olds.
China has also adopted this strategy, even though it is a rapidly ageing country. It clearly distinguishes itself from the UK policy, arguing that vaccinating those in the working age group is a more responsible approach than vaccinating the elderly. In terms of medical ethics, this can be seen as maximising the benefits of vaccines by saving the most life-years rather than the greatest number of lives.
Equity
Not many countries have addressed equity issues directly. One exception is the CDC and National Institute of Health in the United States, which sought an equitable framework for allocation of vaccines given the short supply.
The commissioned report by the National Academies of Sciences, Engineering, and Medicine (NASEM) focused on fairness, transparency and evidence-based policy. To ensure that these criteria were met, priority recommendations were based on each group’s risk of acquiring infection, severe morbidity and mortality, negative social impact and transmission to others.
The report found that the pandemic affected particular minority groups in the United States disproportionately, and recommended that these groups be explicitly addressed in allocating vaccines. The CDC adopted these recommendations in its guidance rather than adopting a single priority criterion, such as age. It is up to individual states to adopt their own policies: Tennessee, for example, has established an order of priority of vaccines for 35 counties in the state based on their social vulnerability index.
The African CDC has issued guidelines that emphasise the importance of fairness, survival of community and social solidarity for developing a framework for allocating vaccines.
The World Health Organization (WHO) has also issued guidelines for fair allocation of vaccines, but these are primarily regarding allocation of vaccines across countries.
Other considerations
While protecting the most vulnerable and protecting key workers (whether in health, logistics, education or public service) have been the primary considerations in priority strategies, these are not the only considerations that have played a role in the allocation of vaccines.
In Indonesia, questions of whether vaccines are halal or not have led to some unwillingness to accept the jab. These arise from the fact that gelatines are required to stabilise the vaccine: major manufacturers have disclosed that they are not using pig products in the vaccines and religious leaders have declared them halal, but scepticism remains. Thus, social media influencers are being offered priority access to vaccines in order to reduce vaccine hesitancy.
For small minority groups facing a high incidence of Covid-19, the survival of their cultures is a crucial consideration. Thus, the Cherokee nation in the United States gives high priority to those who are Cherokee speakers and important for cultural preservation. Indonesia also vaccinated artists and cultural icons in a high-profile event.
Cricket is the main sport in Bangladesh and to participate in international matches as well as start the domestic season, cricketers will be vaccinated first. The strategy of vaccinating professional sports players has not been followed by most other countries.
Finally, most countries are not recommending vaccinations for children. While children do get infected with the virus, the effect on them is less severe than on older cohorts (Goldstein et al, 2020; DeBiasi and Delaney, 2020). Thus, from the viewpoint of reducing severe effects, vaccinating them has remained a low priority.
But schools and universities do play a role in transmission of Covid-19 (Chernozhukov et al, 2021). One new strain has higher infectivity among children and currently in Belgium where schools have been open, 10-19 year olds are the drivers of infection. So going forward, testing whether vaccines are safe for children will be something to consider carefully in order to reduce infections in the population.
Taking stock
Any priority strategy must balance protection against severe illness and mortality with reducing transmission of the disease. Vaccinating 20-49 year olds first would be the most effective strategy to control the spread of Covid-19, as this group is the main driver of infections (Monod et al, 2021). But this would leave the more vulnerable without protection, which could lead to higher overall death rates. In contrast, vaccinating the over-60s will minimise mortality (Bubar et al, 2021).
Protecting the most vulnerable from serious illness or death is a crucial concern and has informed the majority of countries’ vaccine allocation strategies. But minimising overall infections will lessen the severity of the pandemic’s economic impact. This gives some weight to the argument that beyond keeping the health system running, the strategy should be to reduce infections.
One way to balance these different concerns is not to allocate vaccines based on a single criterion as is being done in most countries, but to have a reserve system or categorised priority system where they are allocated to multiple categories with different priorities within each (Pathak et al, 2021). This avoids the problem of upgrading on person’s priority while downgrading someone else’s. A reserve system has already been adopted by at least 11 US states.
An example of a categorised priority system would be to reserve a fifth of vaccines for health and care home workers, a fifth for other key workers including school teachers and law enforcement officers, a tenth for socially disadvantaged and minority groups who have higher Covid-19 mortality than the general population, and the rest for the medically vulnerable, largely assessed on the basis of age.
Conditions within countries – from demographics and healthcare capacity to economic constraints and the socio-political situation – will determine what is the best strategy for each to adopt.
The situation is changing very rapidly and the efficacy of existing vaccines against emerging strains is not fully understood. Covid-19 may become endemic (which means that it would be here to stay), and there may be a need for repeated doses of newly engineered vaccines. Thus, the issue of vaccine priority is likely to persist for some time.
Different countries have adopted vastly different priorities on who should be vaccinated first. These have been decided by specialised committees instituted for this purpose or public health authorities without widespread consultation. There should be open discussions of vaccinating priorities, with consensus developed around what is the appropriate route forward for a country.
Where can I find out more?
- Covid-19: how to prioritize worse-off populations in allocating safe and effective vaccines: Study in the British Medical Journal examines existing frameworks and calls for making a priority of worse-off groups.
- Covid-19 vaccination and prioritisation strategies in the EU/EEA: Report exploring factors that may affect the choice of Covid-19 vaccination strategies.
- Fair allocation of scarce medical resources in the time of Covid-19: Ezekiel Emanuel and colleagues examine fair allocation of medical equipment and interventions.
- Framework for equitable allocation of Covid-19 vaccine: Report from the National Academy of Science, Engineering and Medicine on designing equitable allocation policies for the Covid-19 vaccine that considers at-risk populations.
- Joint Committee on Vaccination and Immunisation: Advice on priority groups for Covid-19 vaccination in the UK.
- The Advisory Committee on Immunizations Practices’ updated interim recommendation for allocation of Covid-19 vaccine: Guidance for federal, state and local jurisdictions in the United States for vaccination planning and implementation.
- WHO SAGE values framework for the allocation and prioritization of Covid-19 vaccination: World Health Organization report on vaccine priorities.
- Covid-19 reserve systems: Resources for implementing reserve systems to balance between different ethical goals.
Who are the experts on this question?
- Aditya Goenka, University of Birmingham
- Parag Pathak, Massachusetts Institute of Technology
- Tayfun Sonmez, Boston College
- Flavio Toxvaerd, University of Cambridge
- Utku Unver, Boston College