Two years on, Covid-19 continues to place a substantial burden on healthcare systems around the world. But the pandemic also provides lessons for policy-makers in building resilient services to protect patients against the threat of future diseases.
There is growing consensus in the scientific community that the Covid-19 pandemic is reaching an endemic stage (Murray, 2022). This means that the disease will remain present in particular populations or regions, as the flu is. But even as this shift takes hold, policy-makers must be prepared for future outbreaks of deadly new viruses.
Response strategies over the past two years have been on a spectrum, ranging from the Swedish approach with almost no restrictions to the extreme zero Covid-19 strategies pursued in China and New Zealand.
A global comparison of the different national prevention, control and response strategies can pinpoint lessons that could help to strengthen countries’ preparedness and reaction to future health challenges.
The pandemic has exposed the limitations of healthcare systems that had previously been classified as high-performing and resilient (El Bcheraoui et al, 2020). Surprisingly, an early analysis suggests that none of the traditional pandemic indices – such as the Global Health Security (GHS) Index, the World Health Organization (WHO) Joint External Evaluation (JEE) and a measure of universal health coverage – explain countries’ performance during the Covid-19 pandemic (Haider et al, 2020).
For example, certain countries that scored poorly on the pandemic preparedness assessment – for example, Burundi, the Dominican Republic and the Philippines – experienced relatively low fatality rates in the initial stages of the pandemic (GHS Index).
Conversely, overall, wealthier countries with more healthcare resources faced a greater burden from Covid-19, in terms of fatality rates, than low-income countries with fewer resources.
The Institute for Health Metrics and Evaluation (IHME) estimates that upper-middle-income and high-income countries (48% of the global population) experienced over half (53%) of the total excess deaths from Covid-19, as of the end of September 2021. This is despite higher-income countries having much higher vaccination rates since the vaccine programmes began (National Preparedness Collaborators).
Different countries’ experiences and outcomes during the pandemic have varied greatly, and the reasons remain complex and unclear. This article explores possible explanations for this ‘epidemiological mystery’ (Mukherjee, 2021). It also looks at the experience of the UK in this context, including what has gone right in its response and what can be learned from its own experience and those of other countries.
How can healthcare performance be measured and compared globally?
A commonly used performance indicator that allows for cross-country comparison is excess deaths. The UK Office for Health Improvement and Disparities defines excess deaths as the number of deaths throughout the pandemic that are above the number expected, based on mortality rates in previous years. IHME estimates excess mortality rates for all countries (Wang, 2021). This is shown in Figure 1.
Figure 1: Estimated excess mortality rate (deaths per 100,000), March 2020 to September 2021
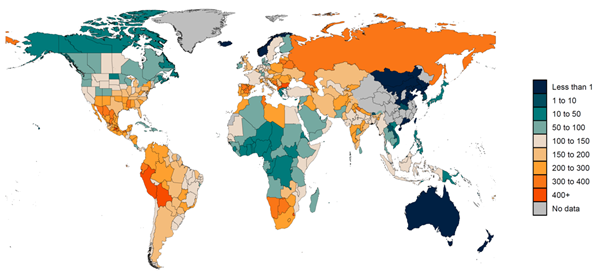
Source: IHME, 2021
To control for differences in population size and age structure between places and different points in time, mortality rates and excess deaths rates are normally standardised. As Covid-19 disproportionately affects older people, and high-income countries have bigger shares of older people than lower-income countries, this method has to be applied to compare countries’ performances globally.
It must be emphasised that cross-country comparisons are inherently difficult due to large disparities in the levels of disease surveillance between countries of different income status. Infection detection rates vary from below 0.1% in some countries to 70% in others (London School of Economics, 2022). Testing equipment, capacity and access vary widely between countries, as do hospital and care capacity. This has led to some countries not reporting hospital admissions at all.
As Covid-19 has become more prevalent – due to more infectious variants such as Omicron – the impact of inadequate distinction in reporting between hospital admissions with Covid-19 versus due to Covid-19 has also become more significant (London School of Economics, 2022).
What explains countries’ performance in the pandemic?
Using age-standardised excess deaths, it is possible to identify which countries have performed well and which ones have not over the past two years. But this measure does not shed any light on what explains their performance. The questions we need to ask are: which approaches have saved more lives and should these be used in the next pandemic?
These questions can be explored by evaluating the impact of different government response strategies across multiple dimensions of healthcare systems. These could include governance and financing mechanisms, community engagement, health service delivery, the health workforce, medical products and technologies, and public health functions. It has been proposed that measuring healthcare systems across these characteristics allows an evaluation of their resilience.
Broadly, resilient healthcare systems have the capacity to prepare for, recover from and absorb shocks, while maintaining core functions and serving the everyday and acute care needs of their communities. Research suggests that healthcare system resilience explains why some countries fared better than others during the pandemic (Haldane et al, 2021).
One analysis of 28 national responses to Covid-19 concludes that there isn’t a single silver bullet to ensure a resilient healthcare system that delivers better performance (Haldane et al, 2021). Nonetheless, highly effective healthcare systems are those that:
- Activate comprehensive responses, which consider and address health and wellbeing in conjunction with social and economic considerations.
- Adapt capacity within and beyond the healthcare system to meet the needs of communities.
- Preserve functions and resources within and beyond the healthcare system to maintain pandemic-related and non-related routine and acute care.
- Reduce vulnerability to catastrophic losses in communities, both in terms of health and wellbeing, as well as individual or household finances.
According to this study, well-performing countries followed whole-of-government approaches and established multi-ministry task forces that could facilitate evidence-informed decision-making.
Other researchers have studied conceptual factors using quantitative methods and found contrary results. For example, one study finds that healthcare capacity indicators, such as hospital beds per capita, were not associated with lower infection fatality ratios (Bollyky, 2022).
Instead, it was lower levels of government corruption and greater levels of trust in government and interpersonal trust that were most associated with fewer infections per capita. This has been observed in Denmark, for example, where trust in the government is very high and infection fatality ratios were lower compared with many other countries.
Similarly, using results from the World Values Survey and European Values Study, researchers found that confidence in public institutions is one of the most important predictors of deaths attributed to Covid-19 (Adamecz-Völgyi and Szabó-Morvai, 2021). Greater confidence in public institutions increases compliance with government mandates, such as social distancing and quarantining, which effectively contributes to the control of viral transmission.
This is in line with other studies finding that less government corruption is associated with greater reduction in mobility, and an increase in Covid-19 policies by governments led to reduced mobility and activity (Bollyky, 2022; McKenzie and Adams, 2020).
Research has also shown that countries’ outcomes during the pandemic were affected by a number of risk factors, including:
- The extent of international and internal travel (Russell et al, 2021).
- The socio-demographic profile of a country (Martín-Sánchez et al, 2021) – specifically, that deaths occurred predominantly in older people and people with health risk factors such as obesity or diabetes (Banerjee et al, 2020; Docherty et al, 2020).
- Social norms and behaviours related to greater risk of disease transmission – countries where social norms are ‘loose’ (for example, where there is greater tolerance for rule breaking) were at greater risk of higher rates of infection relative to those with ‘tight’ social norms (Gelfand et al, 2021). Non-pharmaceutical interventions such as mask mandates and physical distancing measures have shaped the impact of the pandemic.
- A country’s prior experience with epidemics – adherence to government mandates and compliance with these measures may be affected by previous epidemic experiences.
- Inequalities in society – in England, people living in the most deprived areas have, on average, an 80% higher risk of dying from Covid-19 (Public Health England, 2020). People in low-income groups, black and Hispanic people and foreign-born populations have been at a greater risk of dying.
How did the UK fare in comparison with global performance?
The UK has had one of the highest death rates (per 100,000 people) from Covid-19 among countries with a population of over 20 million (Haldane et al, 2021).
During the spring of 2020, the UK had the second highest peak in Europe, at 101.5% of deaths above the five-year average (see Figure 2); Spain was the highest at 142.9%. But the UK’s high fatality rate was only observed in the first wave of the pandemic.
Figure 2: Relative age-standardised mortality rates
Source: Office for National Statistics, National Records Scotland, Northern Ireland Statistics and Research Agency and Eurostat
Note: For all countries where data are available, colour coded by whether the highest peak was in spring 2020 or autumn to winter 2020, UK coloured in dark blue
Looking at deaths of people aged under 65 years, the UK had the highest peak age-standardised mortality rate during the spring of 2020 out of all European countries (Raleigh, 2021). Overall, comparing excess mortality estimates in the first year of the pandemic, the UK ranked seventh out of 22 European countries, with only Spain, Belgium and some East European countries having higher rates.
How has the existing healthcare structure influenced the UK’s performance?
The pandemic has shed light on healthcare systems’ strengths and uncovered structural and chronic vulnerabilities. The UK’s National Health Service (NHS) has been applauded for working under centralised leadership and continuing to provide all treatments free of charge. This included the provision of free Covid-19 tests.
But the pandemic has led to workforce shortages in the NHS, as employees faced excessive workload and burnouts. This especially affected staff from ethnic minority backgrounds, the same communities that were among the most vulnerable to the disease more generally. This indicated the severe issue of structural racism in the UK.
Despite a lot of criticism, the UK was exemplary in some areas, for example:
Innovations in service delivery
With additional financial support – of £48.5 billion – existing NHS public service and charity capacities were expanded, and Covid-19 related treatment services were provided to UK residents free of charge. Hospitals’ infrastructure was optimised by redesigning existing space for clinical use and repurposing wards for Covid-19 patients. This led to an increase in critical care capacity from approximately 4,000 to 7,000 beds. General practitioners also collaborated with clinical commissioning groups to provide consultations remotely so that patients could be triaged before appointments.
Supply chain management
Parallel supply chains were also set up to support the NHS system to distribute medical essentials rapidly. For example, exports of essential medicines, such as insulin and hydroxychloroquine, were banned over fears of domestic shortages. Private companies such as brewers contributed to the production of hand sanitisers by taking the alcohol from their production lines to bolster local and regional supply.
Research and technology
Rapid and up to date genomics sequencing and surveillance was set up. There was also fast and effective Covid-19 vaccine development, led by the University of Oxford, which has had an immense global impact. The UK’s widespread vaccination programme has achieved the highest vaccination rates across European countries.
In addition, free one-to-one support sessions with accredited psychologists or mental health experts have been available to NHS staff. A tool kit was also developed by the NHS to encourage conversations in the workplace about mental and emotional health.
What went wrong?
Several critical arguments have been suggested as explanations for the high Covid-19 fatality rate in the UK, including:
- A delayed and inadequate government response, especially at the start of the pandemic (British Medical Journal, 2020). In line with the slow reaction of the global health community, the UK assumed a ‘wait and see’ strategy with the aspiration of achieving ‘herd immunity’.
- The UK’s borders remained mostly open, with no border policies in place for months. Even when introduced, they were unmonitored and relaxed in comparison with other countries.
- There was a lack of clear leadership and messaging and policy – and decision-makers broke their own rules.
- In 2009, the UK created an independent committee – the Scientific Advisory Group for Emergencies (SAGE) – with the aim of facilitating evidence-informed decision-making. It was hoped that the best available scientific research would be translated into policy during the pandemic. But the credibility of this committee was called into question as political involvement was uncovered.
- In the first instance, the government also treated the virus like a bad flu, not taking the warnings from public health experts seriously. This response undermined the early warnings of scientists.
- The UK failed to protect its health and social workers adequately. During the first national lockdown, health and social care workers lacked appropriate personal protective equipment (PPE), and many were exposed to Covid-19 on wards or in care homes. At this time, there was little to no access to testing. Later, the Covid-19 threat level was downgraded so that a lower level of PPE was required to treat patients – a move that has been condemned by healthcare workers (British Medical Journal, 2020).
- Waiting lists built up as elective treatments had to be cancelled or postponed. Ethnic minority groups, people living in deprived areas and women were disproportionately affected by this, linking to the issue of structural racism (Warner et al, 2021; Burns, 2022).
How can healthcare systems prepare for future shocks?
Less pressure on healthcare systems leads to better performance. Strengthening all aspects of healthcare systems is key to increasing a country’s capacity to respond to the next pandemic. This requires a holistic, multi-sectoral approach and investment in innovation. Even though innovative solutions and quick transformations were put in place during Covid-19, not all are necessarily sustainable.
Countries must develop sustainable healthcare systems that are prepared to respond immediately to a pandemic, and avoid relying on emergency responses such as task-shifting (an approach that aims to optimise the use of the existing healthcare workforce by reallocating highly qualified healthcare workers to other positions that often require less training).
To achieve this, more investment is needed and both power and responsibility should be granted to healthcare leaders during health crises (see a more in-depth discussion here). To make healthcare systems more resilient, an analysis conducted across all OECD countries found that an extra investment of around 1.5% of GDP is required. The largest proportion of the invested funds should be allocated to staffing (Health Foundation, 2022).
Covid-19 has shocked healthcare systems globally. We have learnt that epidemiology and infectiology need a task force dedicated to policy questions around effective resource allocation.
The pandemic has also uncovered structural and chronic vulnerabilities of healthcare systems, which need to be addressed by policy and decision-makers at all levels. For example, the sudden disruption of global supply chains for PPE, essential pharmaceuticals (including sedatives, dialysis fluids and neuromuscular blockers) and medical devices (such as ventilators, infusion pumps and laboratory technologies), alongside a surge in demand for these products, led to many countries experiencing supply shortages (EU Expert Group on Health System Performance, 2020). After a decade of austerity in public spending and years of underfunding, local services were left ill equipped to cope with the pandemic in the UK.
As Covid-19 is thought to become a recurrent disease, we must continue to learn about the most effective prevention and control strategies from other countries. A holistic approach addressing issues that are beyond the national healthcare system needs to be considered to prepare for future shocks. This includes the establishment of more robust supply chains, as well as greater investments in other sectors, such as education.
Where can I find out more?
- How to prevent the next pandemic: Bill Gates discusses lessons from Covid-19 and sets out how governments can collaborate with one another, and private companies, to tackle future health crises.
- How are deaths counted? Report from the King’s Fund.
- Covid-19 Stringency Index: An interactive map showing the level of response to Covid-19, including measures such as school closures and travel bans.
- Covid-19 policy tracker 2020 (England only): The Health Foundation’s timeline of national policy and healthcare system responses.
- A global database of Covid-19 vaccination numbers: From Our World in Data – and how these data are sourced is outlined in an article in Nature.
- Resources on racism in healthcare from the British Medical Journal.
Who are experts on this question?
- Azra Ghani
- David Spiegelhalter
- Joelle Abi-Rached
- Christopher Murray